-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Steinecker Markus, Renger Fabian* and Czirfusz Attila
Corresponding Author: Fabian Renger, Medical Care Centre Dr Renger/Dr Becker Heidenheim, Germany.
Received: August 25, 2024 ; Revised: September 07, 2024 ; Accepted: September 10, 2024 ; Available Online: September 16, 2024
Citation: Markus S, Fabian R & Attila C. (2024) The Financial Impact of the COVID-19 Pandemic in Germany. J Nurs Midwifery Res, 3(2): 1-6.
Copyrights: ©2024 Markus S, Fabian R & Attila C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Introduction: The novel coronavirus (COVID-19), first discovered in China in December 2019, evolved into a serious global pandemic in early 2020. In 2021, its mortality was reduced thanks to vaccinations, and contact restrictions could be scaled back. This led to higher costs in certain cost categories and to upheaval in balance sheets.
Objectives: The aim of this paper is to identify the financial impact of the COVID-19 pandemic on hospitals and to document this impact on the basis of statistical data.
Methodology: Expert interviews, statistical analysis, data processing, depicting the conclusions and linking them to the statistics and information provided by interviewees.
Results: An overall picture emerges of the impact of the novel coronavirus on the profitability and the financial status of hospitals.
Conclusions: A pandemic cannot be tackled effectively by means of organizational measures alone. Infection control, vaccinations and other measures for tackling the pandemic create considerable additional costs for the state and medical facilities, and have a measurable impact on the balance sheet and income statement. Despite the recognized problems with Germany’s personnel and procurement policies, which proved to have little resilience in the pandemic, Germany’s financial policy, with its support of clinics and facilities, appears very balanced in practice.
Keywords: Coronavirus, COVID-19, Pandemic, Balance sheet, Income statement, Expert interviews, Statistical analysis
COST IMPACT OF THE COVID-19 PANDEMIC PER CAPITA
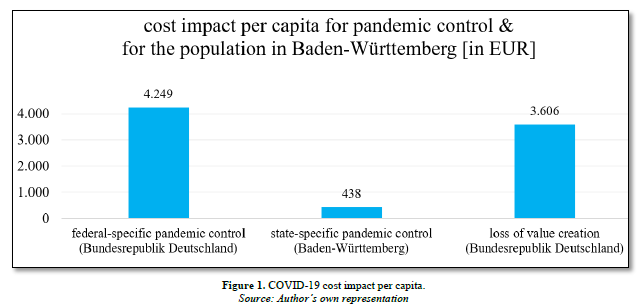
During the COVID-19 pandemic in Germany, top priority was given to protecting the German population. Lockdowns, face masks, curfews, working from home-public life was severely restricted [1]. The aim of these measures was to keep incidence and mortality rates as low as possible. In addition to the problems arising from isolation, this involved considerable additional expenses from an economic point of view [2-3]. In a Federal Ministry of Finance publication from April 2023, one month after the official end of the pandemic, the state expenses at federal level since 2020 were said to be roughly EUR 353.5 billion. As Germany has a population of 83.2 million, this corresponds to EUR 4,249 per capita [4-6]. Additional expenses were incurred at state level. The state of Baden-Württemberg, for example, has incurred additional costs of EUR 4.9 billion in connection with the pandemic since 2020. With the state having a population of 11.2 million, this is equivalent to an additional EUR 438 per capita [6-8]. Overall, this means that a total of EUR 4,687 was spent per capita at federal and state level to tackle the pandemic in Baden-Württemberg. These were not the only costs incurred as a result of the pandemic, however. Value creation was also curtailed. Determining the extent of these losses between February 2020 and February 2023 is not easy owing to the Russia-Ukraine conflict that began in February 2022. Amounts can be determined for the first two years, however. These costs were incurred firstly as the result of production- and transport-related material shortages caused by lockdowns and sickness-related limitations, and secondly because of temporary trade/export restrictions, in particular in relation to medical goods from Asia. On this basis, the German Economic Institute (IW) calculated that the German economy as a whole suffered loss of EUR 300 billion in the first two years [9]. The time period following this is overshadowed by the energy supply shortages and the sanctions arising from the Russia-Ukraine conflict and will therefore not be included in the analysis of the pandemic. In the per-capita analysis, this therefore means an additional sum of EUR 3,606. Accordingly, the countermeasures taken by the federal and state governments and the curtailment to value creation resulted in total costs of EUR 8,293 per capita. The table below provides an illustrated summary of the impact (Figure 1).
SURVEY ON THE FINANCIAL IMPACT OF THE COVID-19 PANDEMIC
In preparation for a survey, 318 clinics and facilities in Baden-Württemberg were contacted, 14 of which stated they were available to participate in expert interviews on the topic of financial issues relating to the COVID-19 pandemic. The interviews were carried out in summer 2022. Almost all facilities confirmed the impact of COVID-19 on costs, albeit to differing degrees and involving different cost types. Under personnel costs such as those for medical staff, nursing staff, medical-technical staff and administration, there were clear negative changes (Figure 2).
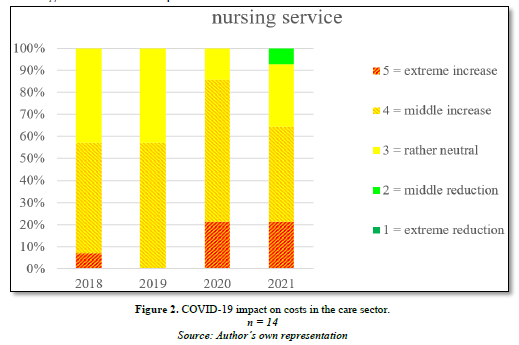
The care sector, which had struggled to attract potential staff even before the pandemic, was further strained. This is also reflected in the graph above. A common reason given was the additional shifts to cover sick leave.
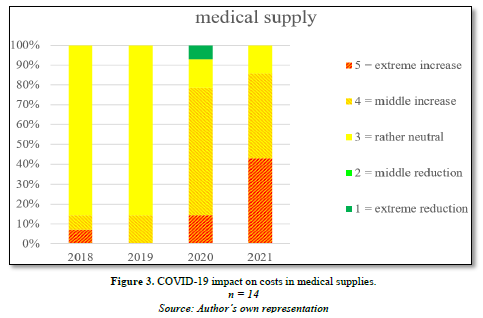
In terms of material costs, food and purchased services increased at some facilities during the pandemic, as did expenses for business and administration and for maintenance covered by nursing charges. The pandemic had a particularly strong impact on medical supplies, as evident in the graph below Figure 3.
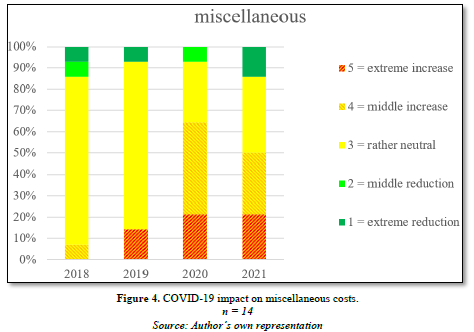
Almost two thirds of the facilities experienced an increase in costs for the cost item miscellaneous.
The cost item ‘miscellaneous’, for which no further details are provided, includes temporary workers who were meant to fill in for absent employees and help address fluctuating workloads and who could not be recruited via the regular labor market. It was pointed out, however, that this section of the labor recruitment market was rapidly depleted, and specialists were then no longer available. The training market is not able to make any additional contribution in this regard because of the latency period and demand. Because of governmental restrictions and a certain level of ambiguity in regulations within Germany and abroad, measures aimed at acquiring staff from abroad require a great deal of patience (Figure 4).
Additional costs were (partially) offset by support measures
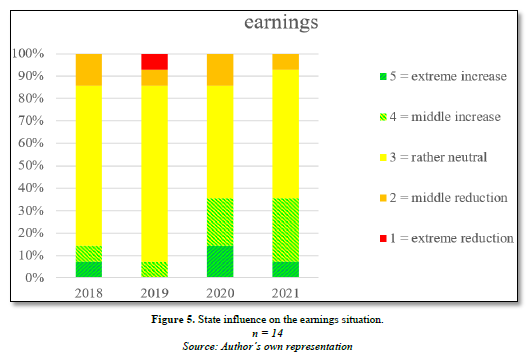
In most clinics, it was possible to keep earnings neutral or even to increase them. In addition to loans and guarantees, this was achieved by means of COVID-19 aid measures such as set payments per bed to cover the fixed costs of empty beds, additional set payments per patient and short-time-working allowances. This enabled many facilities to offset the additional costs incurred (Figure 5).
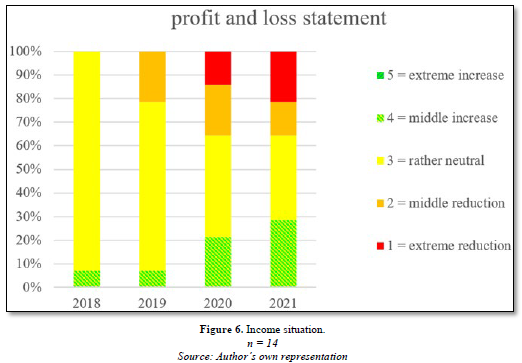
The income situation, on the other hand, is more nuanced. State support was only sufficient to cover the additional expenses and fixed costs in some facilities. Other facilities could not fully offset their losses despite support from the state. This shows that, overall, facilities differed in how well they were able to cope with the pandemic (Figure 6).
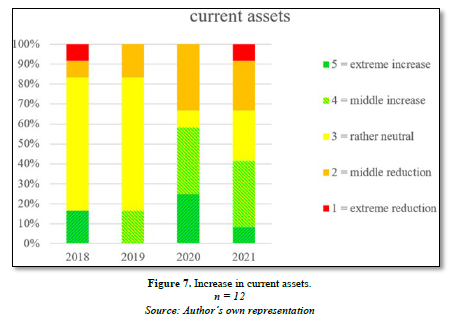
In addition to cost impact, there were also balance sheet implications. On the asset side of the balance sheet, stocks were accumulated. While these initially have no direct effect on profit, they do have a negative impact on cash flow, as the building up of stocks needs to be paid for and funds need to be made available accordingly. Measured against other cost items, however, stock accumulation was not of central importance. As the procurement market was also rapidly exhausted, stocks could only be increased to a limited extent. Other clinics had difficulties in accessing the procurement markets, as the markets had already been exhausted. The accumulation of stocks during the pandemic is shown very clearly in the following graph (Figure 7).
There were differences in how fixed assets developed in the clinics. Some facilities used the COVID-19 period specifically for structural investments in facilities, amenities and additional equipment. For other facilities, fixed assets were reduced overall by depreciation and amortisation (Figure 8).

The liabilities side of the balance sheet includes special items, provisions and borrowed capital as well as equity. There were no noteworthy changes in borrowed capital among the facilities surveyed. Provisions increased in 2020, but decreased again in 2021. The reason for this was that provisions were established at a greater rate at the start of the pandemic. This was partly due to restructuring measures, but partly also due to fears of long-term operating restrictions. The facilities were able to adjust to the pandemic later on, however, so the reason for establishing provisions no longer applied. The special items included funding for capitalized investments or fixed assets, which increased during the pandemic. The total equity situation also improved slightly for many of the facilities surveyed.
CONCLUSIONS AND RECOMMENDATIONS FOR POLICYMAKERS
The clinics and facilities differed in how well they dealt with the pandemic in financial terms. The facilities surveyed did not, however, consider themselves at risk of insolvency. Labour recruitment, which was already in decline before the pandemic, very quickly reached the end of market availability. The same situation was evident in the procurement market for medical supplies. Internal stocks were quickly used up and market stocks were very quickly exhausted. Domestic production, often outsourced abroad in the past, was not able to satisfy demand adequately, and foreign markets largely closed themselves off. It is clear that the reserves and buffer stocks held within Germany are insufficient or non-existent for reasons of cost-efficiency. Maximizing efficiency thus proves to provide little resilience in times of crisis. The clinics and facilities are only able to respond to such limited resource situations as they unfold and work with reduced capacity-despite regrouping because of staff shortages and a ban on visitors owing to a lack of protective equipment. It is therefore recommended that additional skilled workers from overseas be admitted without excessive bureaucracy and that production be brought back to Germany. Building up additional reserves for shortages should also be a goal. Despite all the criticism levelled at Germany’s personnel and procurement policies, Germany’s financial policy appears very balanced. The compensation given to clinics and facilities to ensure that they would survive was not excessive and encouraged the recipients to deal with the limited resources cost-effectively. This is ultimately illustrated by the fact that some facilities achieved better economic results and others achieved worse during the pandemic compared with the period beforehand.
No Files Found
Share Your Publication :